
BETA-THALASSEMIA TREATMENTS
and Iron Chelation
include regular blood transfusions and bone marrow transplants.
How Do Blood Transfusions Help?
Since people with TDT cannot make enough hemoglobin on their own, they require regular red blood cell transfusions in order to treat their anemia and keep them alive. Blood from a donor contains working red blood cells that help treat anemia, facilitate normal growth and activity levels, and improve quality of life. The new blood is able to deliver the oxygen (fuel) that their body needs.
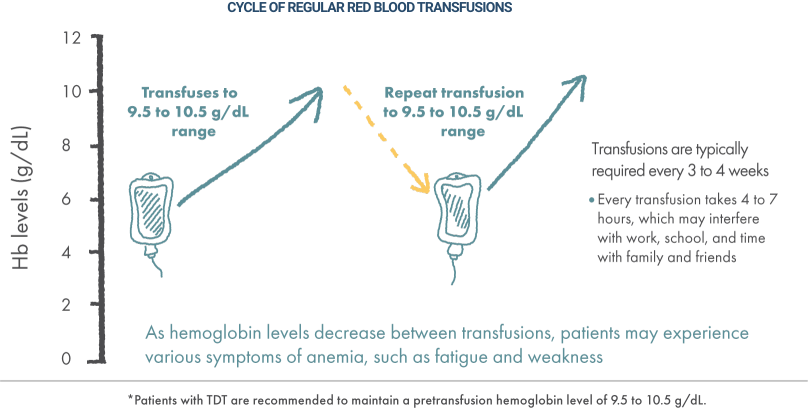
After people with TDT receive a red blood cell transfusion, their hemoglobin levels may go up, and they usually feel good and energized for a period of time. But once their hemoglobin levels begin to decrease and levels get low, they can start to feel tired and weak, which often means it’s time for another transfusion.
To maintain normal levels, they need blood transfusions on a regular basis. It’s important for a person with TDT to stay with a transfusion schedule, as symptoms can progressively get worse over time.
Maintaining Normal Hemoglobin Levels
When receiving a blood transfusion, it’s important to make sure you are achieving near-normal hemoglobin levels. You and your doctor will work together to determine the right timing, transfusion amount, and target adult hemoglobin level for your body.
Guidelines for Transfusions
Guidelines from the Cooley’s Anemia Foundation recommend that the target hemoglobin level be maintained in the 9.5 to 10.5 g/dL range, typically accomplished by administering transfusions every 3 to 4 weeks for most patients.
 SWIPE OR ROTATE
SWIPE OR ROTATE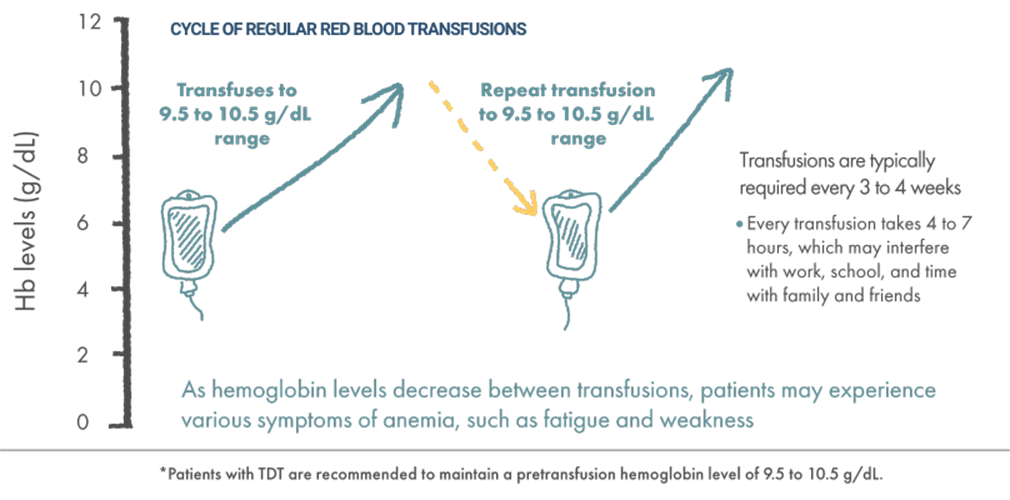
As you age and you go through lifestyle changes, you may need to adjust your timing and target adult hemoglobin levels again. Maintaining a transfusion schedule is a big commitment, but it is necessary for your health. If your body doesn’t get the transfusions it needs, your symptoms could progress from weakness and fatigue to some of the more severe ones listed on the Impact of Beta-Thalassemia page.
Listening to your body and reporting any patterns that you notice (like feeling more tired or less energetic) to your doctor will help you work together to determine a transfusion schedule that works for you. Figuring out the right timing, transfusion amount, and target hemoglobin level for your body may not happen at first, but through a strong partnership with your doctor it can come together over time.
For adults, there is a medication you can pair with red blood cell transfusions to help address some of the symptoms associated with beta-thalassemia.
Iron Overload in Beta-Thalassemia: Side Effect from Regular Blood Transfusions
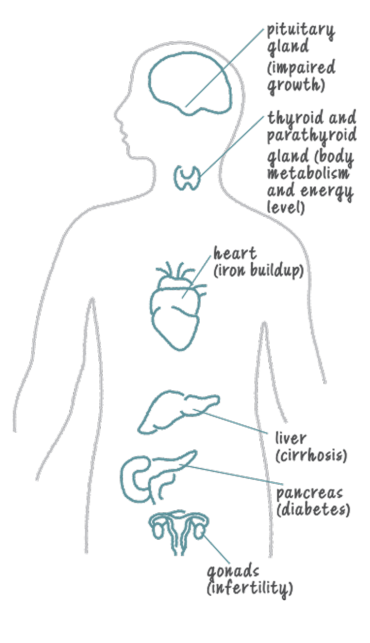
While regular red blood cell transfusions can help manage the symptoms of TDT, they can contain a lot of iron—sometimes more than your body can process on its own. Over time, the iron from transfusions can build up on top of the excess iron that you may have due to beta-thalassemia. This is called iron overload, and the iron collects in organs like your heart, liver, and endocrine systemEndocrine Systemthis system is made up of the glands and organs that produce hormones and release them into the blood, so that they can travel to organs and tissues throughout the body.
Iron overload can make it difficult for these organs to work properly. For example, iron overload in the endocrine system may cause diabetes as well as fertility and other hormonal issues. The iron buildup can also lead to other serious complications, including organ damage and organ failure, if it is not treated effectively.
Monitoring iron levels in the body is an important part of comprehensive TDT care. Iron overload can be monitored through serum ferritinSerum ferritina test used to diagnose and monitor iron overload or iron deficiency testing (a type of blood test). Serum ferritin correlates with how much iron you have stored in your body. A steady decrease in serum ferritin typically indicates a lower amount of iron. However, the measure is not always reliable, as serum ferritin levels may change for a variety of reasons that are not related to iron levels. Magnetic resonance imagining (MRI) is the gold standard for measuring the amount of iron in your organs: liver iron concentration (or LIC)Liver iron concentration (LIC)a way to measure the accumulation of iron in the liver. Elevated levels of iron in the liver may lead to liver disease and damage to the heart for your liver and cardiac T2* (or T2-star) for your heart.
How Can Iron Overload Be Treated?
You may experience iron overload either as a result of beta-thalassemia or from ongoing red blood cell transfusions. Your doctor may treat iron overload with special medications. This kind of treatment is called chelation kee-LAY-shun therapy.
Chelation therapy involves administering a medicine called an iron chelator that binds to the iron in the blood and then works to remove it through urine and/or bowel movements. Chelation therapy can be administered a number of different ways, including intravenous (IV), subcutaneous pump, or in oral form.
It is important that you develop a regular routine for taking your medication for chelation therapy throughout your life, as even short periods without chelation can have damaging effects on your body. Talk to your doctor about managing your iron levels and keeping your organs as healthy as possible.
Please note that the information here about treatment is for general educational purposes only. You should always speak to your doctor about the possible risks and side effects associated with treatments for beta-thalassemia.
DID YOU KNOW?
Heart disease caused by iron overload was once the leading cause of death in people with thalassemia, and remains one of the most common complications.
Staying motivated
Josephine has been living with beta-thalassemia since she was a child and receives frequent blood transfusions, but she doesn’t let that stop her from pursuing her passions.
“As someone who has been living with this illness for over 30 years, I know firsthand how difficult it is to balance.”
Josephine
actual beta-thalassemia patient
 This website is developed by bluebird bio, Inc. and is intended for residents of the United States who are 18 years and older.
This website is developed by bluebird bio, Inc. and is intended for residents of the United States who are 18 years and older. 